

From Zero to Thousands: PrEP rollout in Cambodia
A new push for prevention
As part of the chapter “A new push for prevention”, we tell the story of Cambodia’s efforts to expand the provision of PrEP in the country.
SCROLL DOWN
“PrEP is really critical for me since my partner lives with HIV and we cannot maintain condom use every time,” said Hay Seiha, one of the more than 3000 people who have started taking Pre-Exposure Prophylaxis (PrEP) in Cambodia.
He gets the medicine at the weekends, so it doesn’t interfere with his work at a marketing company. “For me PrEP is easy to take, and I had no side effects at all. I can do my daily work as usual while having some extra protection against HIV,” he added.
It has been more than a decade since the life-saving preventive HIV medicine, PrEP, has shown its effectiveness but global rollout has been slow. Cambodia is one of the few countries that has recently expanded access to PrEP across the country.
Dr Kret Setha, who works at the Family Health Clinic Tuol Kork Health Center in Phnom Penh, explained how the center has had many new walk-in clients either after seeing social media campaigns or because they have been referred by a community-based organization.

“Our clinic does not require clients to go through a registration desk so people can come and see counsellors directly for screening and PrEP services,” he said.
Confidentiality, flexible hours and adapted services for key populations have been critical to attracting potential clients.
Thearo (who did not wish to give a last name) had heard about the clinic from his co-workers at an all-male massage parlor. He came to the clinic for an HIV and sexually transmitted diseases check-up. After a counselling session, he decided to try the new medicine.
“I have many sexual clients due to the nature of my job, so PrEP helps to prevent HIV infection when taking it regularly,” he said. He looks forward to the long-acting PrEP either orally or through injection because he fears forgetting to take his pills.
According to Dr Ouk Vichea, Director of the National Center for HIV/AIDS, Dermatology and STDs, 70% of people enrolled in PrEP are men who have sex with men, followed by transgender women and female entertainment workers. The center within the Ministry of Health has been leading PrEP rollout along with UNAIDS, WHO, FHI 360/EpiC Project, NGOs and several community-based organizations. “Cambodia’s PrEP target is to have 10 000 people enrolled by 2023,” said Dr Vichea.
However, despite the country’s efforts, COVID-19 delayed the rollout of PrEP and prevented the government and partners from organizing event launches, trainings and workshops for service providers and potential clients.
Two main challenges remain: attracting new clients and keeping them on PrEP.

For Dr Setha quality counseling is the game-changer to get more people enrolled and sticking to this preventive medicine.
“Following up with a phone call and providing friendly, immediate feedback to questions and inquiries makes all the difference,” he said.
So far, most PrEP clients live in Phnom Penh, so UNAIDS and partners have worked hand in hand designing rollout, capacity needs and implementation in other provinces.
“To generate demand for PrEP, we helped community-led organizations raise awareness among at risk communities via social media, special events and in-person outreach,” said Polin Ung, UNAIDS Cambodia Strategic Intervention Adviser.
“It has not been easy. Service providers have not always been keen on distributing PrEP and people have not flocked to it, but mentalities are changing,” he explained.
He thinks that evidence-based advocacy helped Cambodia to adopt PrEP rollout quite quickly. Now it’s a question of local acceptance and demand creation.
“Community engagement in the design, delivery and expansion of PrEP services are key to its long-term success,” he said.
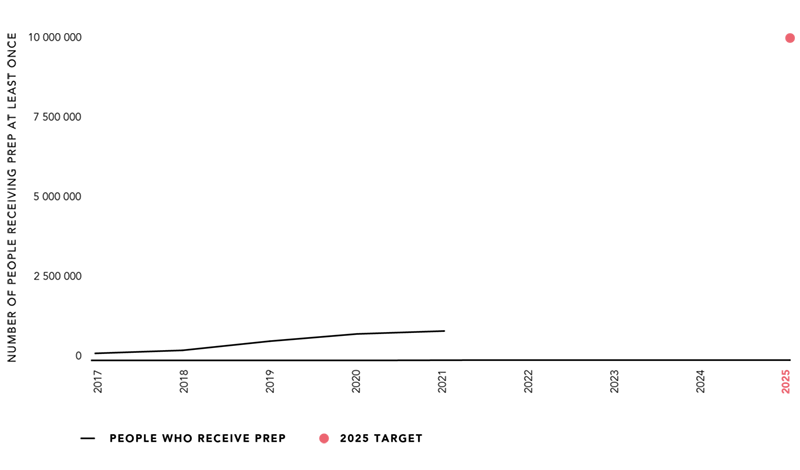
In 2021, more than 1.6 million people worldwide were receiving oral PrEP. People who used PrEP at least once during the reporting year increased approximately two-fold from 820 000 in 2020 to 1.6 million in 2021. The increased PrEP use in 2021 occurred despite the COVID-19 pandemic and represents a continuation of the increased use of PrEP since 2016, although it remains well short of the 2025 target of 10 million people.
Until recently, PrEP use was concentrated in high-income countries. The last two years, however, have seen a pronounced uptake of PrEP in eastern and southern Africa. In 2021, South Africa, Kenya and Zambia drove the rapid uptake of PrEP in eastern and southern Africa, with more modest progress made in other countries in the region. In other regions of low- and middle-income countries, by contrast, minimal progress has been made in expanding the access and use of PrEP.
All pictures: UNAIDS/Todd Brown
HIV prevention programmes across all regions are incomplete, missing priority populations, or they are too small to have a decisive impact. In this chapter, read more about:
